This article provides accessible advice for doctors encountering aesthetic (non-surgical cosmetic) complications in the emergency department or primary care setting. We recognise that aesthetic medicine represents a private healthcare sector with little to no representation in the undergraduate curriculum. Clinicians working in the emergency department or primary care setting are therefore likely to lack experience with the management of complications related to non-surgical aesthetic treatments. Nonetheless, patients who do develop concerns or complications following these interventions may present or be referred to NHS services. An understanding of how to assess, diagnose and treat such complications within the NHS setting is therefore required in order to protect patient outcomes.
Contents
INTRODUCTION TO AESTHETIC PROCEDURES
GENERAL RED FLAGS IN AESTHETIC PATIENTS PRESENTING TO THE EMERGENCY DEPARTMENT
“LUMPS OR BUMPS” POST-INJECTABLE TREATMENT
INTRODUCTION TO AESTHETIC PROCEDURES
Aesthetics, also known as ‘non-surgical cosmetic medicine’, encompasses a wide range of minimally-invasive medical procedures including botulinum toxin injections, dermal fillers, and thread lifts. In the UK, where the practice of aesthetics is relatively unregulated, there has been a rise in associated complications and rates of attendance to emergency departments.1 Commonly, these issues arise from treatments by unqualified individuals using unlicensed products in substandard working conditions.2-8
The most serious potential complications that may present to the emergency department generally occur after filler injections and thread lifts.7
GENERAL RED FLAGS IN AESTHETIC PATIENTS PRESENTING TO THE EMERGENCY DEPARTMENT
- Patients who are systemically unwell
- Visual disturbance
- Severe pain, pallor and delayed capillary refill in the surrounding region to that which was treated
- Patients injected with unknown/unlicensed product
- Patient who are immunocompromised or have an unstable co-morbidities
- Medications that may increase the risk of infection: steroids, chemotherapeutic agents, immunosuppressant drugs, and disease-modifying drugs.
WHAT ARE DERMAL FILLERS?
Dermal fillers are injectable products that are used to restore volume and enhance structure in the face or body. The most common type of dermal filler is made of hyaluronic acid, which can be dissolved with hyaluronidase enzyme in the case of dermal filler being injected into or around a blood vessel and compromising blood flow. This is a complication known as vascular occlusion. Hyaluronidase may be available in some hospital ITUs/HDUs, but is not typically stocked in emergency departments.
There are other dermal fillers known as semi-permanent or stimulatory fillers, which cannot be dissolved by hyaluronidase. Unfortunately, there are also hundreds of unregulated or unknown filler brands that can be cheaply acquired online without being sourced from legitimate pharmacies.
“LUMPS OR BUMPS” POST-INJECTABLE TREATMENT
There is a wide differential for an unknown “lump or bump” post-injectable treatment. When a patient presents to the emergency department with a an unknown “lump” after a filler treatment, the most important thing is to decide whether or not the lump is infected and necessitates IV antibiotics or surgical intervention.
Differentiation Guidelines for Post-Injectable “Lump or Bump”
Differentiating between the types of “lumps or bumps” following injectable treatments is critical for appropriate management:
- Type I Reaction: Quick onset of symptoms such as angioedema or urticaria, typically occurring within minutes to hours post-injection. The incidence of Type I reactions and anaphylaxis is low, but should be manged via the Advanced Life Support (ALS) algorithm.9
- Haematoma: A localised swelling filled with blood, often associated with bruising and tenderness at the injection site.
- Oedema: Generalised swelling at or around the injection site, which is usually non-tender and diffuse, and can be managed conservatively.
- Malar Oedema: Injections into the infraorbital hollow are associated with malar oedema, which can be refractory to treatment and develop into a chronic problem.10, 11
- Tyndall Effect: Light scattering from particles in a dermal filler injected too superficially can lead to a blueish discolouration, particularly around the periorbital and perioral region.12
- Nodules (Inflammatory and Non-inflammatory): Nodule formation can result from various factors including infection, biofilm formation, or a Type IV hypersensitivity response.10, 13 ‘Nodule’ is a descriptive term, rather than a diagnosis, and the aetiology is still poorly understood.14
- Infective Aetiology/Abscesses: These present as fluctuant, erythematous, and warm lumps, indicating possible infection or pus collection.15
- Biofilm Formation: This may not present as a classic infection initially; instead, it can cause a waxing and waning of inflammation over time.
- Type IV Reaction/granulomas: These delayed hypersensitivity reactions can lead to inflammation that either fades over time or becomes chronic, often without the immediate dramatic symptoms of Type I reactions. Granulomas are the hallmark of chronic inflammatory Type IV responses and are composed of multinucleated giant cells.16
When to refer to plastic or maxillofacial surgery
- Patients with signs of severe infection or sepsis.
- If abscess formation is suspected, incision and drainage will be necessary.
- NB: In the context of lumps and bumps, those without signs of active infection are not normally referred or admitted – they should be signposted back to their aesthetic practitioner for management.
Assessment & Recognition of Infected “Lump or Bump” needing admission
- On palpation a fluctuant, erythematous, warm mass
- Bedside observations ?sepsis
- FBC, U+Es, CRP, clotting
- Blood cultures if signs of sepsis
- Send wound swab if open wound
- Ultrasound may be useful to characterise the mass – but this is often not indicated in the acute setting
Management of infected lumps / bumps following cosmetic injectables
- Initiate empirical antibiotic therapy according to local antimicrobial guidelines
- Acute infections are typically due to pathogens commonly seen on the skin: Staphylococcus aureus, Staphylococcus epidermidis, and Streptococcus pyogenes15
- Surgical consultation for incision and drainage of abscess
- Consideration of admission for intravenous antibiotics in cases of severe or rapidly progressing infections
VASCULAR OCCLUSION
A vascular occlusion (VO) is a medical emergency that can result from cosmetic injectables such as dermal fillers. A VO indicates the obstruction of blood flow due to either the injection of filler into a blood vessel as an embolus or the compression of a vessel by a bolus of dermal filler adjacent to it.17 A VO can result in necrosis of a particular region of tissue supplied by the obstructed blood vessel. If the occlusion as presented at the point of necrosis, careful wound debridement and care is critical.17 Blindness can also occur as a result of dermal filler-associated VO through the obstruction of vessels such as the central retinal artery or ophthalmic artery.
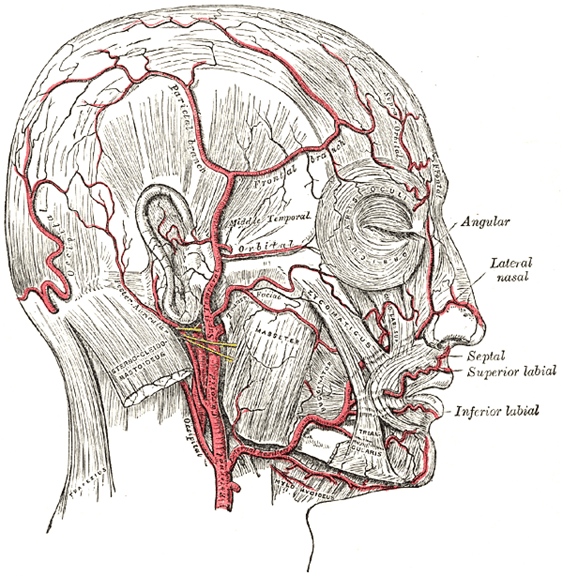
Figure 1. The facial artery. From Gray’s Anatomy.
Recognition of vascular occlusion:
- Immediate pallor / discolouration of the skin post-injection
- Severe and persisting pain out of proportion to the procedure
- Coolness, blanching and delayed capillary refill (>2s)
- Livedo reticularis: a lace-like pattern of blood vessels visible on the skin
- Doppler ultrasound can help assess blood flow if available
If suspected VO advise the patient that immediate action is required to prevent lasting damage
Immediate Management of a Suspected VO (See Quick Guide for Algorithm):
- Warm compresses, massage, and regular checking and documentation of capillary refill
- 300mg Aspirin STAT followed by 75mg OD until resolution12, 18
- Consider GTN paste12
- Note: may cause disproportionate venous dilation and compromise deeper blood flow17
- Initiate the high-dose pulsed hyaluronidase protocol18
- 1500u hyaluronidase in 1mL NaCl or 1-2% lidocaine
- Flood the suspected pathway of the vascular occlusion
- Treat to effect rather than use a specific dose
- Repeat hyaluronidase every 15-20 min until capillary refill <2s
When to involve the plastic or maxillofacial surgery registrar:
- If there are signs of vascular compromise to the tissues
- Late presentations with tissue necrosis and/or infection
Assessment & recognition of late-onset vascular occlusion needing admission
- Signs of tissue extensive necrosis or infection requiring debridement and IV antibiotic cover
- FBC, U+Es, CRP
- Blood cultures if signs of sepsis
- Send wound swab if open wound
Management
- Initiate empirical antibiotic therapy according to local antibiotic guidelines
- Surgical consultation for the potential need of wound debridement/care
- Consideration of admission for intravenous antibiotics in cases of severe or rapidly progressing infections
VISUAL LOSS
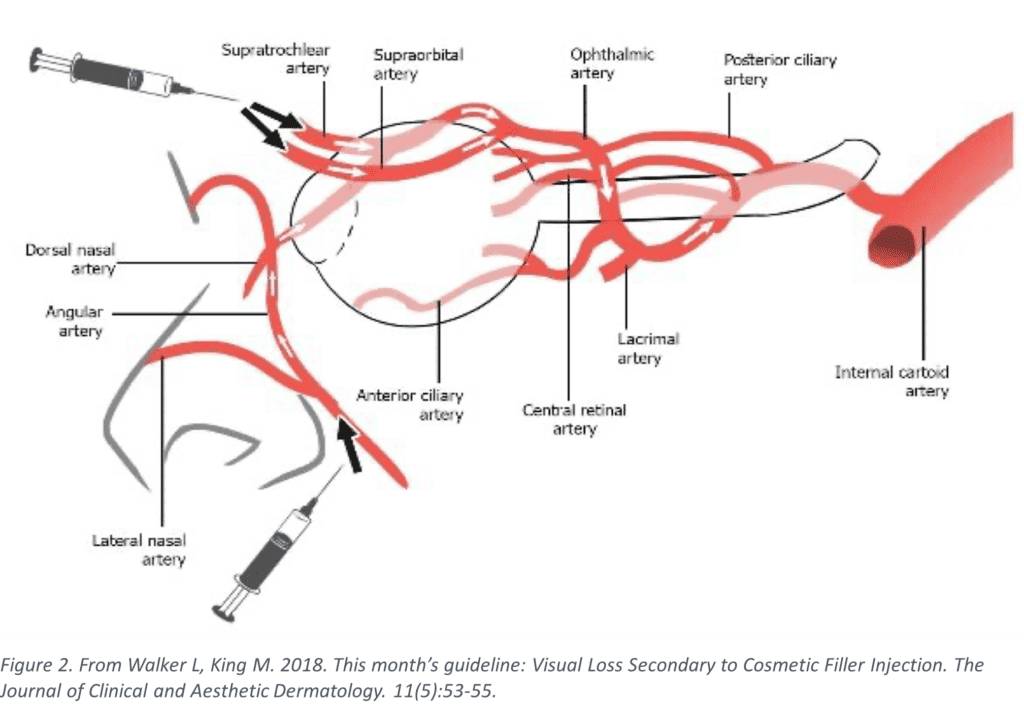
Visual loss post-injection is a rare but catastrophic event that may result from vascular occlusion leading to central retinal artery occlusion or direct compression of the optic nerve (Figure 2). It is important for clinicians to recognise and initiate management immediately as the general consensus is that interventions are time critical.19
Red Flags:
- Severe pain with visual disturbance or blindness immediately post-injection19
- Rapid afferent pupillary defect (RAPD)
- Ptosis or ophthalmoplegia19
- Blurred vision19
- Ocular, periorbital, periocular, orbital, eye pain or headache with nausea and vomitting19
When to refer to the ophthalmologist:
- Immediate referral to an ophthalmologist if any visual symptoms are present
- Ideally, any patient with visual symptoms post-injectables should present directly to a specialist eye hospital
Assessment & Recognition of Visual Loss needing admission:
- Consider the original site of hyaluronic acid placement and possible anatomical connections to ocular blood supply
- Check visual acuity from worst to best: no light perception, light perception, crude motion, counting fingers19
- Document pupillary reactions and eye movements
- Intraocular pressure should be assessed
Management:
- Place the patient in the supine position with the head raised 15-45 degrees19
- A rebreather bag can be utilised to produce hypercapnia and hypoxia in order to increase retinal blood flow and cause vasodilation19
- Ocular massage may be performed by trained clinicians to potentially dislodge the occlusion12
- Pressure applied on closed eye for 5s, released for 10s, in a pulsatile manner for 5 minutes
- 3 sets total can be performed
- Timolol 0.5% drops (to reduce intraocular pressure)19
- Consider soluble aspirin 300mg STAT19
- Consider sublingual glycerol trinitrate (GTN) for vasodilatation19
- High-dose pulsed hyaluronidase protocol (see under VO section)
- Flood the suspected pathway of filler (Figure 3)
- Urgent transfer to specialist eye unit
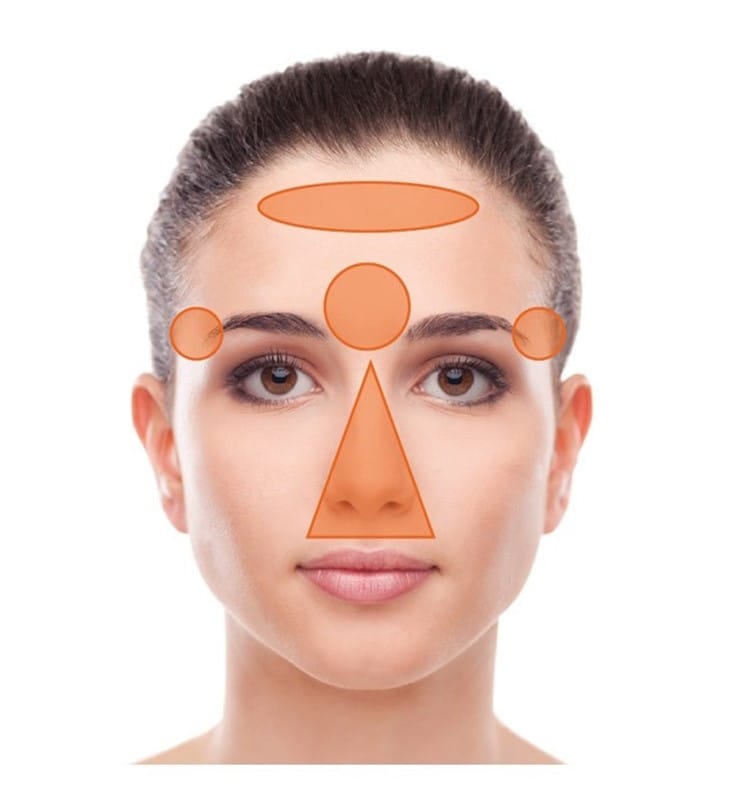
Figure 3. Areas of dermal filler injection associated with increased risk of blindness. From Chatrath V, Bannerjee PS, Goodman G, Rahman E. Soft-tissue filler-associated blindness: a systematic review of case reports and case series. Plast Reconstr Surg Glob Open.
WHAT ARE THREAD LIFTS?
Thread lifts are minimally invasive procedures that practitioners perform under local anesthesia. These procedures involve inserting temporary sutures under the skin to lift and tighten sagging tissues. The threads used often consist of materials that encourage collagen production. Threads can be either absorbable or non-absorbable, with non-absorbable threads associated with higher complication rates.
In the UK, the most commonly used threads are absorbable, typically made of PDO (polydioxanone) threads, followed by PLA (poly-L-lactic acid) threads and PCL (polycaprolactone) threads.
VISIBLE THREADS AND EXTRUSION
Visible threads and extrusion occur with superficial or incorrect placement of threads, causing them to dimple the skin, appear visible or be palpable.22 Older patients are at increased risk of this complication.21 This typically becomes evident two to four weeks after the procedure, once the initial inflammatory process has subsided.23
When to Involve the plastic or maxillofacial surgery registrar:
- Visible or palpable threads causing patient distress
- Evidence of thread extrusion and superficial placement
Management:
- Initiate massage therapy to facilitate thread integration or manually release tension in barbed threads, if appropriate21, 24
- Barbed threads should be massaged in the opposite direction of placement24
- If the tip of the thread is palpable and accessible, attempt careful extraction and trimming under sterile conditions, provided you are skilled and competent in this technique22
- Be cautious as thread breaking may occur if excessive traction is applied, leading to retraction of the remaining thread fragment21
- Where the practitioner is not experienced or confident in managing the complication, refer the patient for surgical removal of the threads, especially in cases of severe extrusion or if the threads are causing significant distress
INFECTED THREADS
Thread lift procedures, while generally safe, can result in complications such as infection.25 Although rare, infection is the most common reason for the removal of threads.21 Infected threads can lead to serious consequences if not promptly identified and managed.26
When to involve the plastic surgery registrar:
- Patients with signs of severe infection or sepsis
- If there is evidence of a spreading infection or abscess formation
- Intractable infection will require thorough removal and debridement21
Assessment of infected threads needing admission:
- Examination for localized warmth, erythema, and tenderness along the thread trajectory
- Persistent redness, swelling, and pain at the site of thread insertion
- Pus or discharge at the entry or exit points of the threads
- Fluctuant collections indicating abscess
- FBC, U+Es, CRP, clotting
- Blood cultures if signs of sepsis
- Send wound swab if open wound
Management
- Initiate empirical antibiotic therapy according to local antibiotic guidelines and dress the site25
- Surgical consultation for the potential removal of infected threads and drainage of any associated abscess
- Consideration of admission for intravenous antibiotics in cases of severe or rapidly progressing infections
CONCLUSION
In the rapidly evolving field of aesthetic medicine, the ability to effectively manage complications is crucial. While this article has provided a concise guide to identifying and addressing some of the most common post-procedural complications in the emergency department setting, hands-on experience and continuous education remain paramount. We strongly encourage clinicians to further their expertise and confidence in managing aesthetic complications through comprehensive training.
APPENDIX OF TERMINOLOGY
Ablative laser resurfacing: Ablative laser resurfacing involves the use of a laser to remove the outer layers of the skin (epidermis) and heat the underlying skin (dermis). This process stimulates the growth of new collagen fibres, resulting in improved skin texture and firmness. [See CO2 and erbium lasers]
Abscess: A collection of pus.
Aesthetic Medicine/Non-Surgical Cosmetic Medicine: This branch of medicine includes all medical procedures aimed at improving the physical appearance and satisfaction of the patient through non-invasive to minimally invasive cosmetic procedures.
Alexandrite Laser: A light source pumps an alexandrite crystal to produce a specific wavelength of light, typically in the infrared range of 755 nm. It is mainly known for its applications in hair removal and treating pigmented skin lesions due to its effective targeting of melanin.
Autologous Fat Transfer: In this procedure, a practitioner transfers fat from one area of the body to another, typically to enhance or augment the area where the fat is injected.
Barbed threads: Threads used in cosmetic procedures that have barbs or cones to lift and secure the subcutaneous fat and muscle, providing a lifting effect. [See cog threads]
Biofilm Formation: The accumulation of microorganisms on a surface, forming a complex structure that can lead to chronic infections.
Biostimulator: Substances used in cosmetic treatments that stimulate the body’s natural processes to produce collagen or other elements, leading to rejuvenation of the skin or tissues.
Body contouring: A range of aesthetic procedures that reshape and alter the human body to enhance its appearance, including procedures to eliminate or reduce excess skin and fat.
Botulinum toxin Type A injections: Injections used in cosmetic and medical procedures that temporarily paralyse muscles, used to treat wrinkles and other conditions.
Buccal fat removal: A cosmetic procedure that involves the surgical removal of buccal fat pads in the cheeks to create a more contoured facial appearance.
Calcium hydroxylapatite: A naturally occurring mineral form of calcium apatite is used in fillers. [See semi-permanent filler, stimulatory filler, Radiesse.]
Carboxytherapy: A non-surgical cosmetic treatment which uses injections of carbon dioxide gas beneath the skin to improve circulation, encourage collagen production, and enhance skin elasticity.
Chemical Peels: Procedures that apply a chemical solution to the skin, causing it to exfoliate and eventually slough off. The new skin is usually smoother and less wrinkled. Chemical peels vary in strength and can treat various skin conditions, including acne, hyperpigmentation, and fine lines.
CO2 laser resurfacing: A cosmetic procedure using a carbon dioxide laser to remove layers of damaged or wrinkled skin. It promotes skin regeneration, leading to smoother, younger-looking skin. It is effective in treating scars, warts, and deep wrinkles.
Cog threads: Synonymous with barbed threads, these are sutures used in cosmetic procedures to lift and support sagging tissue. [See barbed threads]
Collagen injections: A cosmetic procedure involving the injection of collagen into the skin to restore lost volume and improve the appearance of aging skin. Popular in the previous decades, hyaluronic acid fillers have largely replaced this now.
Cosmeceuticals: A hybrid of cosmetics and pharmaceuticals, these are cosmetic products with bioactive ingredients purported to have medical benefits.
Cryolipolysis A non-invasive body contouring procedure that uses controlled cooling to freeze and eliminate fat cells without surgery. Commonly known as fat freezing, its uses is to reduce fat bulges in specific areas. [See CoolSculpting]
Cut threads: Threads that have barbs cut into them.
Exosomes: Extracellular vesicles that play a role in cell communication, also explored in skin rejuvenation treatments
Deoxycholic acid: A bile acid naturally found in the body which breaks down and absorbs fats in our diets. Injected in nonsurgical treatments to break down and absorb fat. [See fat-dissolving, Kybella, Aqualyx.]
Dermabrasion: A surgical procedure that involves the controlled abrasion (wearing away) of the upper layers of the skin with a rapidly rotating device. Dermabrasion smoothens the skin and removes scars, wrinkles, and other skin imperfections.
Dermal Fillers: A general term for biocompatible materials injected into the skin to restore volume, smooth lines, soften creases, or enhance facial contours.
Dermaplaning: A skin treatment that uses an exfoliating blade to skim dead skin cells and hair from the face. It aims to make the skin’s surface smooth, youthful, and radiant. Additionally, it removes peach fuzz on the face.
Diplopia: Double vision.
Electrolysis: A method of removing individual hairs from the face or body by destroying the growth centre of the hair with chemical or heat energy. A very fine probe is inserted into the hair follicle, and then an electric current is applied to destroy the follicle, resulting in permanent hair removal. Another use of electrolysis is on benign skin lesions.
Erbium (Er:YAG) laser resurfacing: A less invasive skin resurfacing procedure that uses an erbium-doped yttrium aluminium garnet (Er:YAG) laser. It removes superficial and moderately deep lines and wrinkles on the face, hands, neck, or chest with minimal burning of surrounding tissue.
Fat dissolving: Acosmetic procedure involving the injection of substances (like deoxycholic acid) into body fat to break it down and absorb it into the body, thereby reducing localised fat deposits. [See Aqualyx, Kybella]
“Fox Eye” threads: Threads used in a cosmetic procedure aimed at lifting the outer corner of the eye to create an elongated and slightly lifted appearance, resembling the “fox eye” makeup trend.
Fractional laser resurfacing: A skin resurfacing procedure that uses a laser to deliver a microscopic column of energy to create zones of injury on the skin.
Granuloma:An aggregation of macrophages that form in response to chronic inflammation.
Hair transplants: A surgical technique that moves individual hair follicles from a part of the body called the ‘donor site’ to a bald or balding part of the body known as the ‘recipient site’. It’s primary use is to treat male pattern baldness.
Haematoma: A localised swelling filled with blood, often associated with bruising and tenderness.
High-Intensity Focused Ultrasound (HIFU): A non-invasive therapeutic technique that uses ultrasonic waves to heat tissue. In cosmetic applications, HIFU is used for skin tightening and lifting by inducing collagen production in the targeted tissue layers.
Hydrafacial: A medical-grade facial rejuvenation treatment that cleanses, detoxifies, exfoliates, extracts, and hydrates the skin in a non-invasive process. It combines multiple skin treatments in one.
Hydroquinone: A prescription skin-lightening agent used to treat hyperpigmented areas by decreasing the formation of melanin in the skin.
Hyaluronic acid: A glycosaminoglycan distributed widely through connective and epithelial tissue. Commonly used in aesthetic medicine as a soft tissue filler.
Hyaluronic acid fillers: Temporary fillers made of hyaluronic acid. They can be dissolved with hyaluronidase.
Hyaluronidase: An enzyme used to dissolve hyaluronic acid fillers in cases of complications like vascular occlusion or visual loss.
Hyperhidrosis: A medical condition characterized by excessive sweating, significantly more than the body requires for temperature regulation. It can affect specific areas or the entire body and often impacts the hands, feet, underarms, or face. Treatment can be done with botulinum toxin type A.
Infected Threads: Complication arising from thread lift procedures, where the threads become infected.
Injectable Treatments: Procedures involving the injection of substances for cosmetic or therapeutic purposes.
Intense pulsed light (IPL): The use of multiple wavelengths of light to improve the appearance of the skin. IPL can treat a range of skin conditions, including sun damage, age spots, freckles, rosacea, and broken capillaries. It is also used for hair removal.
Jessner’s Peel: A type of chemical peel that uses a combination of salicylic acid, lactic acid, and resorcinol in an ethanol base. This makes it useful to rejuvenate the skin by removing the upper layers, improving skin texture, reducing dark spots, and treating acne.
Laser skin rejuvenation: A cosmetic procedure using laser technology to improve the appearance of the skin.
Laser hair removal: A cosmetic procedure that uses laser technology to remove unwanted hair by targeting the melanin in hair follicles. The laser emits a light that is absorbed by the pigment in the hair, damaging the follicle enough to inhibit future hair growth.
Lip lift: A cosmetic surgical procedure that shortens the space between the nose and the top of the lip (the philtrum) to increase the amount of pink lip that is visible.
Livedo reticularis: A lace-like pattern of blood vessels visible on the skin, often indicating vascular issues. This is a sign of vascular occlusion.
Malar oedema: Swelling in the cheek area, typically resulting from injections into the infraorbital hollow.
Melasma: A common skin condition characterized by brown or grey-brown patches, typically on the face. Melasma occurs much more often in women than men, and is often associated with hormonal changes, such as pregnancy or birth control pills, and sun exposure.
Microcurrent therapy: A cosmetic treatment that uses low-level electrical currents to stimulate facial muscles, essentially giving the face a “workout.” It is used for anti-aging purposes, aiming to tone muscles.
Microdermabrasion: A non-invasive cosmetic procedure that uses a mechanical medium for exfoliation to remove the outermost layer of dead skin cells from the epidermis.
Microneedling: A cosmetic procedure that involves repeatedly puncturing the skin with tiny, sterile needles to induce the production of collagen and elastin.
Monofilament Threads: Threads consisting of one long filament.
Moulded Threads: Threads that have barbs placed onto them.
Multifilament Threads: Threads consisting of multiple filaments, often braided together.
Nd:YAG Laser: A type of laser commonly used in medical and cosmetic procedures. The Nd:YAG laser emits light at a wavelength of 1064 nm, making it suitable for a variety of applications, including hair removal, skin rejuvenation, and the treatment of vascular lesions and pigmented lesion.
Nefertiti neck lift: A non-surgical procedure named after the Egyptian Queen Nefertiti, known for her elongated, smooth neck. It involves injecting botulinum toxin along the lower jawline and down the neck along the platysma muscle, leading to a more defined jawline and smoother neck.
Nodules: Nodule is a swelling or lump in the tissue and is a descriptive term, rather than a diagnosis. Nodule formation can result from various factors, including infection, biofilm formation, or a Type IV hypersensitivity response.
Non-ablative laser: Non-ablative laser resurfacing, on the other hand, works by heating up the underlying skin tissue (dermis) without harming the surface (epidermis). [See Nd:YAG, Alexandra, pulsed-dye lasers]
Non-fractional laser: A type of laser treatment that delivers a solid, uninterrupted beam of light to the treated area. Unlike fractional lasers, which create micro-injury zones, non-fractional lasers treat the entire area uniformly. They are typically used for more intensive skin resurfacing, treating wrinkles.
Non-surgical nose job (NSR): The use of dermal fillers to straighten and define the nose. High-risk area of filler associated with blindness with several case studies documented in the literature.
Nutraceuticals: A broad term that encompasses products derived from food sources with extra health benefits in addition to their basic nutritional value. Nutraceuticals can include dietary supplements, fortified food products, or herbal products.
Oedema: Generalised swelling at or around the injection site, usually non-tender and diffuse.
Ophthalmoplegia: Paralysis or weakness of the eye muscles. It can present with blurry vision, strabismus, diplopia, and difficulty in eye movement.
“O-shot”: A non-invasive procedure that uses platelet-rich plasma (PRP) extracted from the blood to improve the health and vitality of the vagina. It encourages the body’s stem cells to produce new tissue. This thickens vaginal tissue to heighten sensitivity thanks to increased blood flow.
Permanent filler: Fillers made of materials that cannot be absorbed or broken down by the body and involve fibrogenesis and collagen production. Materials include silicone, polymethylmethacrylate, and polyacrylamide.
Photodynamic therapy: A treatment that uses photosensitising drugs and light to kill cancer cells and other diseased cells. The drug becomes activated by a specific wavelength of light and creates a form of oxygen that kills nearby cells. It’s used for various medical and cosmetic purposes.
Photorejuvenation: A cosmetic treatment that uses lasers, intense pulsed light (IPL) or photodynamic therapy to improve the appearance of skin.
Plasma fibroblast therapy: A non-surgical skin tightening procedure that uses high energy discharge to make a small wound in the skin, this encourages fibroblasts to repair the skin and maintain firmness. [See Plasmage, PlasmaIQ].
Platelet-rich plasma (PRP): A concentrate of platelet-rich plasma protein derived from whole blood, centrifuged to remove red blood cells. It has a high concentration of growth factors and is used in various medical and cosmetic treatments to promote wound healing, skin rejuvenation, and hair growth.
Polyacrylamide: A synthetic polymer formed from acrylamide subunits and a non-absorbable volumising gel. Often used to treat HAART-related lipodystrophy syndrome (facial wasting) in HIV patients. [See permanent fillers].
Polycaprolactone (PCL): This biodegradable polyester has a long history of use in biomedical applications. In aesthetic medicine, practitioners use PCL as a bioresorbable scaffold in dermal fillers. PCL stimulates natural collagen production over time and is known for its long-lasting effects in skin rejuvenation and volume restoration. This material finds use in threads [See Happy Lift] and fillers [See Ellanse].
Polydioxanone (PDO): Polydioxanone (PDO) is a synthetic, biodegradable polymer widely used in medical applications, particularly for producing absorbable sutures. In aesthetic medicine, practitioners use PDO for thread lift procedures, inserting fine threads under the skin to lift and tighten sagging tissues. This material is used in threads [See Mint, Intraline].
Polylactic-co-glycolic (PLGA): A biodegradable functional polymer made from lactic acid and glycolic acid. Used in threads. [See Silhouette]
Poly-L-lactic Acid (PLLA): PLLA is a synthetic, biodegradable, biocompatible polymer of lactic acid. It’s used in biomedical applications such as sutures, orthopaedic devices, and drug delivery systems. PLLA can increase dermal thickness and stimulate collagen production through a subclinical inflammatory response. This material can be used in fillers [See Sculptra].
Polymethylmethacrylate: PMMA is a synthetic polymer derived from methyl methacrylate.
Polymethylmethacrylate microspheres (PMMA): Manufacturers create these transparent thermoplastic microbeads known for their high impact and heat resistance and good tensile and flexural strength. Practitioners use PMMA microspheres in semi-permanent fillers to treat medium-to-deep wrinkles, folds, pitted scars, and thin lips augmentation [See Bellafil].
Polynucleotide: A polynucleotide is a biopolymer composed of nucleotide monomers bonded covalently in a chain. Increasingly, practitioners in aesthetic medicine are utilizing polynucleotides for their regenerative properties.
Ptosis: Drooping of the upper eyelid.
Pulsed-dye laser: Laser which uses an organic dye mixed in a solvent as a lasing medium. A high energy source of light excites the dye molecules stimulating them to emit radiation. Often used to treat cutaneous vascular lesions, warts, angiofibroma and pyogenic granulomas.
Q-switched lasers: Q-switched lasers are a type of laser technology. The “Q” in Q-switched stands for “quality factor,” a measure of the efficiency of the laser. Q-switched lasers are special lasers known for their ability to produce high-intensity laser beams in very short pulses. The mechanism involves temporarily storing energy in the laser medium and then releasing it in a short, intense burst.
Radiofrequency: A measurement representing the oscillation rate of electromagnetic radiation spectrum or waves. In aesthetic procedures the use of an electromagnetic device that generates heat can stimulate the production of collagen, elastin and new skin cells in skin tightening treatments.
Radiofrequency microneedling: An advanced skin treatment technique that synergistically uses the mechanical action of microneedles with the thermal energy of radiofrequency waves. This combination aims to enhance skin rejuvenation and address various skin concerns more effectively than microneedling alone.
Rapid Afferent Pupillary Defect (RAPD): A condition where pupils respond differently to light stimuli shone in each eye.
Sclerotherapy: Treatment to improve the appearance of varicose and spider veins (and other vascular malformations). Involves the injecting of a chemical solution directly into the veins causing the vein walls to swell and stick together sealing them to stop the blood flow.
Semi-permanent filler: A type of filler (also known as stimulatory filler) with increased longevity in the tissues in comparison to hyaluronic acid fillers. These produce a foreign body reaction and stimulate collagen production. They are immunologically inert and are metabolised to CO2 and water by the body. They do not cause the immediate volume enhancement but results build up over time.
Silicone: A synthetic substance that has been used as permanent filler in liquid silicone form for decades [See permanent fillers].
Skin Booster: A skin booster is a cosmetic treatment designed to hydrate, rejuvenate, and improve the overall quality of the skin. It typically involves the use of hyaluronic acid injections or other nourishing substances. [See Profhilo]
SMAS: (Superficial Muscular Aponeurotic System): SMAS refers to a layer of tissue in the face that plays a critical role in facial aesthetics and surgical procedures like facelifts.
Smooth threads: Threads that do not contain barbs.
Stimulatory fillers: A semi-permanent filler.
Strabismus: Misalignment of one or both eyes.
Subcision: A cosmetic procedure used to treat scars and wrinkles. It involves breaking up fibrous tissue bands that cause skin depressions.
Tear trough filler: A treatment involving the injection of dermal fillers under the eyes. It aims to reduce dark circles or hollows, creating a more refreshed and rejuvenated appearance.
Thread Lifts: Minimally invasive procedures involving the insertion of temporary, absorbable sutures under the skin to lift and tighten sagging tissues.
Tretinoin: A topical prescription medication derived from Vitamin A, used to treat acne, reduce wrinkles, and improve skin texture. It speeds up cell turnover and stimulates collagen production.
Trichology: The scientific study of hair and scalp health, focusing on hair growth, hair loss, and associated scalp conditions.
Trichloroacetic acid (TCA) peel: A type of chemical peel used in skin treatments, involving the application of trichloroacetic acid to remove dead skin cells, reduce scars and wrinkles, and improve overall skin texture.
Type I Reaction: Immediate hypersensitivity reaction such as angioedema or urticaria, occurring shortly after injection.
Type IV Reaction: Delayed hypersensitivity reactions leading to chronic inflammation and granuloma formation.
Tyndall effect: Blueish discoloration of the skin due to light scattering from particles in a dermal filler injected too superficially.
Ultrasound reduction: The use of lower frequency ultrasonic waves to form bubbles around fat deposits under the skin. While the bubbles burst, the interstitial and lymphatic systems drain the fat deposits.
Ultrasound skin tightening: The use of high-frequency sound waves to heat deeper layers of the skin, the cellular damage promotes collagen production resulting in tighter, firmer skin.
Vascular Occlusion (VO): Obstruction of blood flow due to the injection of filler into a blood vessel or compression by dermal filler.
APPENDIX OF TRADE NAMES
Allergan: Allergan Aesthetics is a pharmaceutical company and subsidiary of AbbVie that develops, manufactures, and markets a portfolio of brands and products including facial injectables and body contouring. It is primarily known for its brands Botox (botulinum toxin), Juvederm (HA filler), and CoolSculpting.
Aliaxin (HA-Derma): A brand of hyaluronic acid dermal fillers.
Alluzience (Galderma): A brand of botulinum toxin type A.
Anchor Plus (Croma Pharma): A brand of barbed polydioxanone(PDO) thread with a double-arrow shape.
Aquamid: A brand of permanent filler made of polyacrylamide.
Aqualyx: A solution containing deoxycholate used for non-surgical reduction of localized fat under the skin.
Asclera: A brand name for a sclerosing agent used in the treatment of varicose and spider veins.
Azzalure (Galderma): A brand of botulinum toxin type A.
Belotero (Merz): A brand of hyaluronic acid dermal fillers.
Bellafil (Suneva Medical): A type of semi-permanent filler consisting of polymethylmethacrylate (PMMA) microspheres in a smooth collagen gel.
BodyTite: A minimally invasive procedure using radiofrequency energy to firm and contour the body by tightening loose skin and reducing fat.
Bocouture (Merz): A brand of botulinum toxin Type A. Known as Xeomin in North America.
Botox (Allergan): A brand of botulinum toxin Type A. It is so well-known it has become synonymous with the treatment.
Cellfina: A non-surgical treatment that targets cellulite via microneedling subcision to break up the dimpling of the skin.
Chroma Pharma: A pharmaceutical company with a comprehensive, minimally invasive aesthetics portfolio. It is primarily known for its Saypha (HA filler) and Letybo (botulinum toxin) brands.
CoolSculpting: A branded, non-invasive cosmetic procedure that reduces fat deposits through controlled cooling. It is a form of cryolipolysis, targeting and freezing fat cells without damaging surrounding tissue.
CryoPen: A handheld device used in cryotherapy to treat skin lesions such as warts, moles, and skin tags by applying extreme cold to destroy abnormal tissue.
CryoSuccess: A portable device used for cryotherapy, specifically designed for the treatment of small skin lesions using nitrous oxide.
Cutera: A company that manufactures laser and other light-based aesthetic systems for hair removal, skin rejuvenation, and other cosmetic procedures.
Daxxify: A novel type of botulinum toxin type A reporting a potentially longer duration of action compared to other botulinum toxin products.
DermaFrac: A micro-needling treatment combined with deep tissue serum infusion, used for skin rejuvenation, treating fine lines, and improving skin texture.
Dysport (Galderma): A brand of botulinum toxin type A. It is known as Azzalure in the European Union.
Ellanse (Sinclair): A stimulatory filler made of polycaprolactone (PCL) homogeneously suspended in a custom aqueous gel carrier of carboxymethylcellulose (CMC).
Emsculpt: A non-invasive body sculpting procedure that uses high intensity focused electromagnetic technology to induce muscle contractions, leading to muscle building and fat reduction in areas like the abdomen and buttocks.
Endymed INTENSIF: A form of radiofrequency microneedling.
E.P.T.Q. (Nordic Medical): A brand of hyaluronic acid dermal filler.
Evolus: A performance beauty company known for its brands Nuceiva/Jeuveau (botulinum toxin).
Galderma: Galderma is a pharmaceutical company specialising in dermatological treatments and skincare products. It is primarily known for its brands Restylane (HA filler), Azzalure/Dysport (botulinum toxin), Alluzience (botulinum toxin), and Sculptra (stimulatory filler).
Halo Laser: A hybrid fractional laser used for skin resurfacing treatments. It combines ablative and non-ablative wavelengths to improve skin texture, tone, and appearance, addressing issues like sun damage, wrinkles, and scars.
Happy Lift: A brand of PCL threads.
HYAcorp (Forma Medical): A brand of hyaluronic acid dermal fillers.
Hydrafill: A brand of hyaluronic acid dermal fillers.
Intraline: A brand of hyaluronic acid dermal fillers and threads.
Jeuveau: A brand of botulinum toxin type A. Known as Nuceiva in the UK.
Juvederm (Allergan): A brand of hyaluronic acid dermal fillers.
Kybella: An injectable treatment used to reduce submental fat, commonly known as a double chin. The active ingredient is deoxycholic acid.
Lanluma (Sinclair): A brand of injectable poly-L-lactic acid (PLLA) used for enhancing and sculpting the body by stimulating collagen production.
Letybo (Croma Pharma): A brand of botulinum toxin type A.
Lumenis: A global developer and manufacturer of laser and energy-based technologies for aesthetic, surgical, and ophthalmology applications.
M22: A modular multi-application platform for the treatment of over 30 skin conditions and hair removal. It’s developed by Lumenis and uses Intense Pulsed Light (IPL) technology.
MaiLi (Sinclair): A brand of hyaluronic acid dermal fillers.
Matexlab: A company known for producing aesthetic medicine products, particularly in injectable fillers and other skin treatments.
Merz: Merz Pharma is a parent company of independent businesses in the fields of aesthetic medicine, therapeutic medicine, and wellness and beauty products. It is primarily known for its brands Belotero (HA filler), Bocouture (botulinum toxin), and Radiesse (stimulatory filler).
Mint: A brand of barbed PDO monofilament threads.
Morpheus 8: A fractional skin treatment that combines microneedling with radiofrequency energy to remodel and contour the face and body, improving skin texture, reducing wrinkles, and promoting collagen production.
Neauvia Organic (MatexLab): A brand of hyaluronic acid dermal fillers.
Nuceiva (Evolus): A brand of botulinum toxin Type A. Known as Jeuveau in North America.
Plasma IQ: A device used for non-surgical blepharoplasty (eyelid tightening) and skin rejuvenation. It uses plasma energy to create micro-injuries on the skin, stimulating natural regeneration and tightening.
PlasmaPen: A cosmetic tool used for non-invasive skin treatments. It employs plasma energy to reduce wrinkles, tighten saggy skin, and improve overall skin texture.
Plasmage: A device that uses fractional plasma technology to perform non-invasive treatments for eyelid lifting, wrinkle reduction, and removal of skin imperfections.
Princess (Croma Pharma): A brand of polydioxanone(PDO) thread
Profhilo: An injectable skin remodelling treatment containing uncrosslinked hyaluronic acid. It is designed to hydrate the skin from within and improve skin tone, texture, and elasticity.
Radiesse (Merz): An injectable dermal filler that contains CaHA microspheres suspended in an aqueous carboxymethylcellulose gel carrier. Radiesse is the only FDA-approved CaHA filler brand.
ReLIFE (Menarini): A brand of hyaluronic acid dermal fillers.
ResurFX: A non-ablative fractional laser skin resurfacing system used for skin rejuvenation, addressing issues like scars, wrinkles, and stretch marks.
Revanesse A range of hyaluronic acid-based dermal fillers designed for anti-aging treatments, including reducing wrinkles and enhancing facial contours.
Revolax: A brand of hyaluronic acid dermal fillers.
Restylane (Galderma): A brand of hyaluronic acid dermal fillers.
Saypha (Chroma Pharma): A brand of hyaluronic acid dermal fillers.
Sculptra (Galderma): A type of stimulatory filler made of poly-L-lactic acid (PLLA).
Silhouette Soft: Poly-lactic-co-glycolic acid (PLLA/PLGA) threads used in aesthetic procedures, composed of polylactic acid monofilament with absorbable cones.
Sinclair: A pharmaceutical company that develops, manufactures, and distributes dermatological products for facial aesthetics. It is primarily known for its brands MaiLi (HA filler), Ellanse (PCL filler), Silhouette Soft (threads).
Skinpen: A medical-grade, state-of-the-art microneedling device used to treat acne scars, stretch marks, fine lines, and improve the skin’s overall appearance by stimulating collagen production.
Stylage (Vivacy): A brand of hyaluronic acid dermal fillers.
Teosyal RHA (Teoxane): A brand of hyaluronic acid dermal fillers.
Teoxane: Teoxane Laboratories is a company that produces hyaluronic acid dermal fillers and dermocosmetic products. It is primarily known for its brand of Teosyal RHA fillers.
Thermage: A non-invasive radiofrequency therapy that can smooth, tighten, and contour the skin for an overall younger-looking appearance, effective on the face, neck, eyes, and body.
Thermavein: A cosmetic treatment used for removing spider veins and vascular blemishes using thermocoagulation.
Tixel: A novel thermal fractional skin rejuvenation system that uses heat to create controlled micro-injuries in the skin, stimulating collagen production and aiding in skin tightening and texture improvement.
Ultherapy (Merz): A non-invasive treatment that uses focused ultrasound energy to lift and tighten the skin on the face, neck, and chest, promoting collagen production and resulting in a more youthful appearance.
Vampire facial: A trademarked cosmetic procedure involving microneedling followed by the application of platelet-rich plasma (PRP) extracted from the patient’s own blood, aimed at rejuvenating the skin and promoting healing.
Viscoderm Hydrobooster (HA-Derma): A product used for skin biorestructuring and deep hydration, known for its hyaluronic acid content that aids in improving skin elasticity and reducing superficial wrinkles.
Vivacy: Laboratories Vivacy is a French company that specializes in designing and manufacturing hyaluronic acid-based dermal fillers and skincare products, including the Stylage line of filler.
Xeomin (Merz): A brand of Botulinum toxin type A. Known as Bocouture in the European Union.
QUICK GUIDE
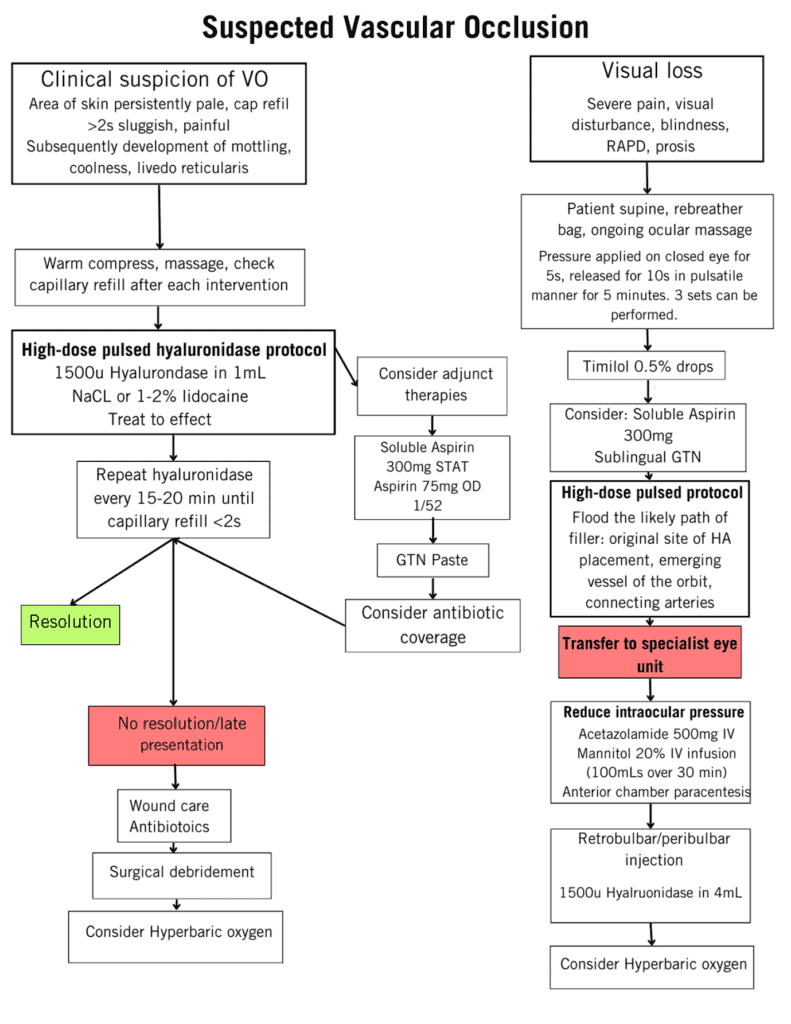
Figure 4. Protocol for vascular occlusion and visual loss. Adapted from Claudio D. New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events. Aesthetic Surgery Journal. 2017 & Walker L, Convery C, Davies E, Murray G, Croasdell B. Consensus Opinion for The Management of Soft Tissue Filler Induced Vision Loss. J Clin Aesthet Dermatol. 2021;14(12):E84-e94
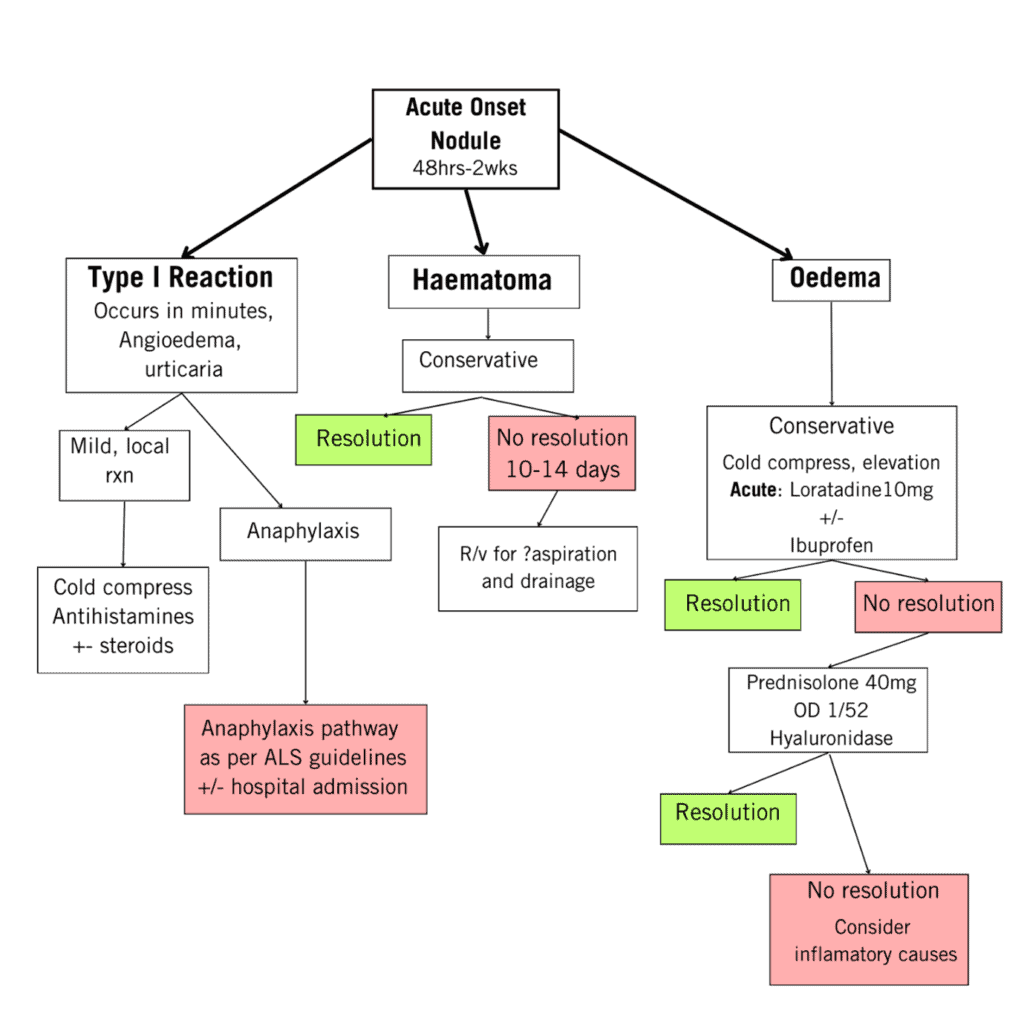
Figure 5. Protocol for the management of acute onset “lump or bump” post-filler injection. Adapted from Davies E, King M. Management of Acute Skin Infections. J Clin Aesthet Dermatol. 2017;10(2):E5-E and Diwan Z, Trikha S, Etemad-Shahidi S, Virmani S, Denning C, Al-Mukhtar Y, et al. Case Series and Review on Managing Abscesses Secondary to Hyaluronic Acid Soft Tissue Fillers with Recommended Management Guidelines. J Clin Aesthet Dermatol. 2020;13(11):37-43.
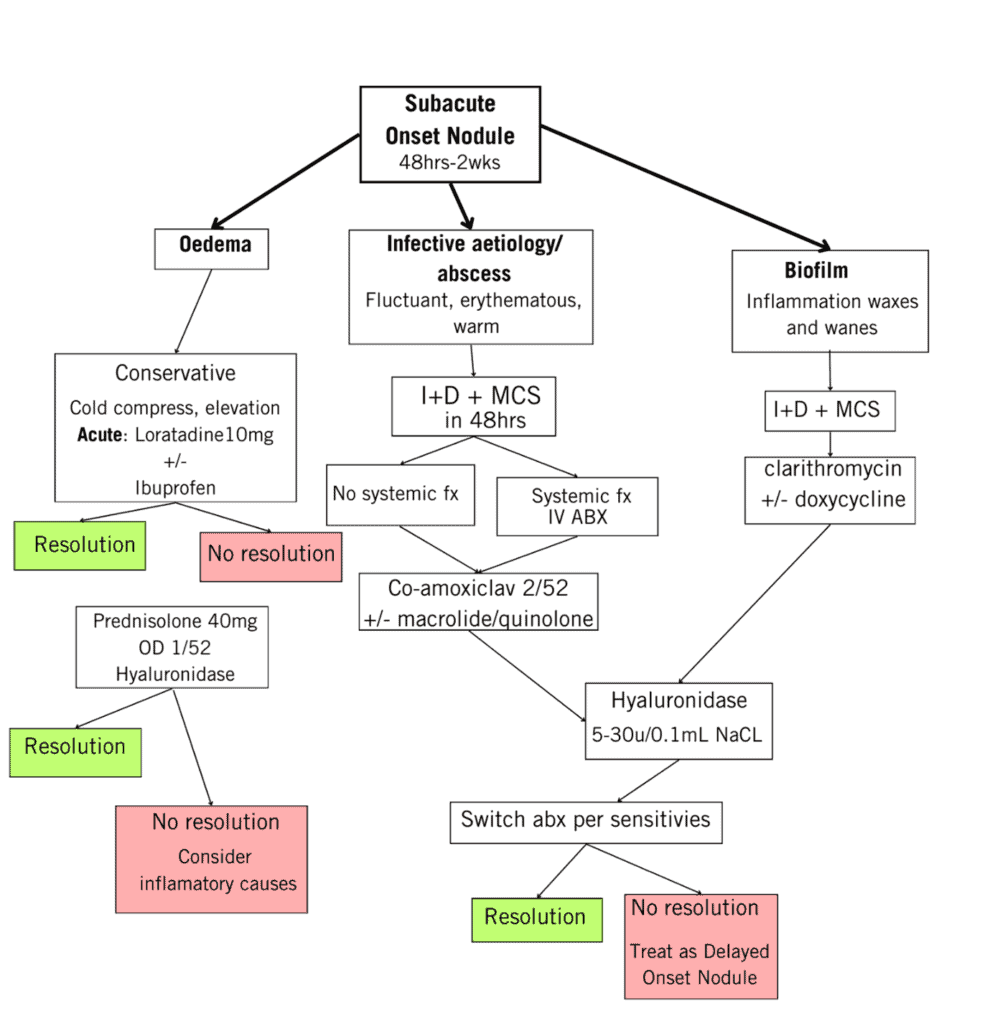
Figure 6. Protocol for the management of subacute onset “lump or bump” post-filler injection. Adapted from Davies E, King M. Management of Acute Skin Infections. J Clin Aesthet Dermatol. 2017;10(2):E5-E and Diwan Z, Trikha S, Etemad-Shahidi S, Virmani S.
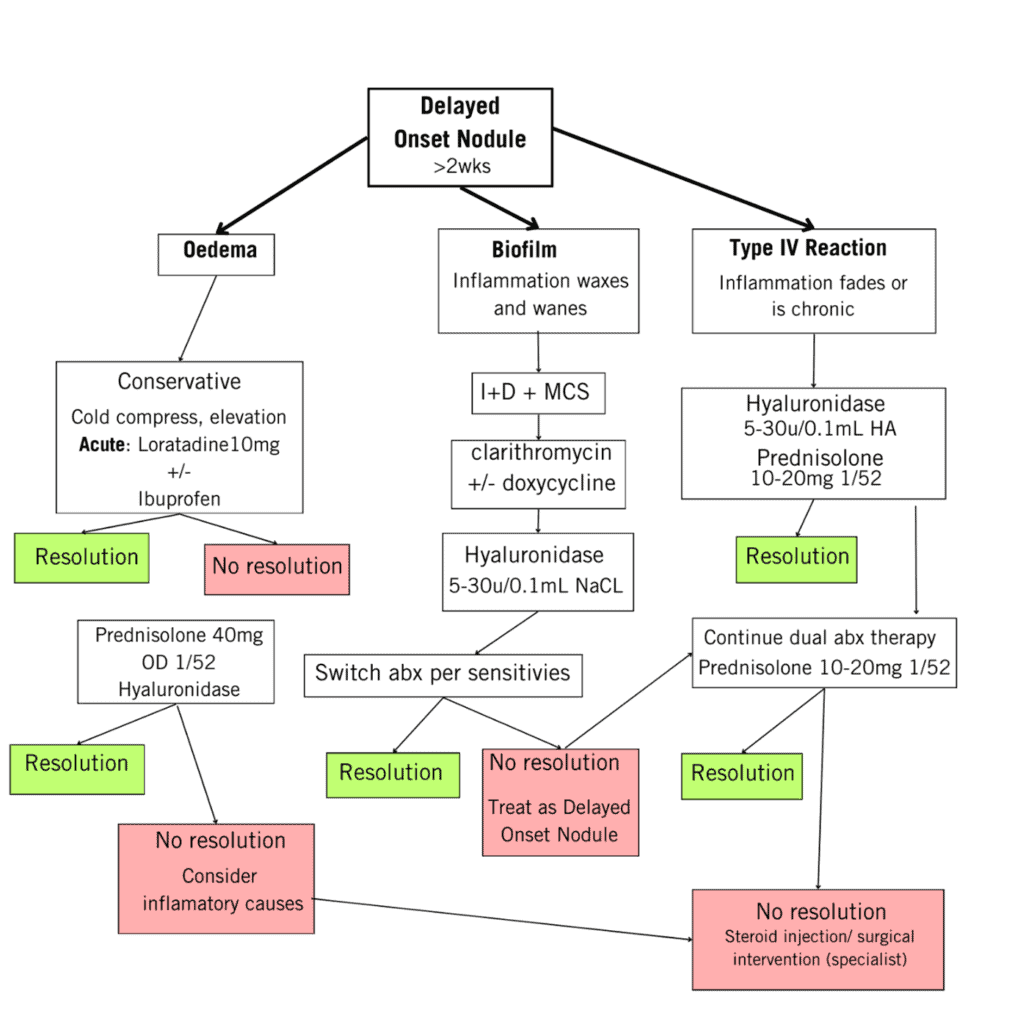
Figure 7. Protocol for the management of delayed onset “lump or bump” post-filler injection. Adapted from Davies E, King M. Management of Acute Skin Infections. J Clin Aesthet Dermatol. 2017;10(2):E5-E and Diwan Z, Trikha S, Etemad-Shahidi S, Virmani S.
REFERENCES
1. Urdiales-Galvez F, Delgado NE, Figueiredo V, Lajo-Plaza JV, Mira M, Moreno A, et al. Treatment of Soft Tissue Filler Complications: Expert Consensus Recommendations. Aesthetic Plast Surg. 2018;42(2):498-510.
2. Blanchard J, Palmer J, Ali E, Cheng L. Complications of Self-Injected Facial Fillers: A Treatment Conundrum in the UK. Case Rep Surg. 2019;2019:2041839.
3. Rauso R, Nicoletti GF, Zerbinati N, Lo Giudice G, Fragola R, Tartaro G. Complications Following Self-Administration of Hyaluronic Acid Fillers: Literature Review. Clin Cosmet Investig Dermatol. 2020;13:767-71.
4. Ono S, Hyakusoku H. Complications after self-injection of hyaluronic acid and phosphatidylcholine for aesthetic purposes. Aesthet Surg J. 2010;30(3):442-5.
5. Coskuner ER, Canter HI. Desire for penile girth enhancement and the effects of the self-injection of hyaluronic Acid gel. J Cutan Aesthet Surg. 2012;5(3):198-200.
6. Raoof N, Salvi SM. Self-injection of dermal filler: an underdiagnosed entity? Br J Dermatol. 2015;172(3):782-3.
7. Berthold R, Berthold R, Claudio D. Understanding, Avoiding, and Managing Severe Filler Complications. Plastic and Reconstructive Surgery. 2015.
8. Save Face. Consumer Complaints Report 2017-2018. 2018.
9. UK Resuscitation Council. Adult Advanced Life Support Guidelines. Resuscitation Council (UK); 2023.
10. Chiang YZ, Pierone G, Al-Niaimi F. Dermal fillers: pathophysiology, prevention and treatment of complications. J Eur Acad Dermatol Venereol. 2017;31(3):405-13.
11. Mustak H, Fiaschetti D, Goldberg RA. Filling the Periorbital Hollows With Hyaluronic Acid Gel: Long‐term Review of Outcomes and Complications. Journal of Cosmetic Dermatology. 2017.
12. Aesthetic Complications Expert Group. Guidelines for the Managemeent of Complications in Aesthetic Practice2018.
13. Ledon J, Savas J, Yang SS, França K, Camacho ID, Nouri K. Inflammatory Nodules Following Soft Tissue Filler Use: A Review of Causative Agents, Pathology and Treatment Options. American Journal of Clinical Dermatology. 2013.
14. Convery C, Davies E, Murray G, Walker L. Delayed-onset Nodules (DONs) and Considering their Treatment following use of Hyaluronic Acid (HA) Fillers. J Clin Aesthet Dermatol. 2021;14(7):E59-E67.
15. Diwan Z, Trikha S, Etemad-Shahidi S, Virmani S, Denning C, Al-Mukhtar Y, et al. Case Series and Review on Managing Abscesses Secondary to Hyaluronic Acid Soft Tissue Fillers with Recommended Management Guidelines. J Clin Aesthet Dermatol. 2020;13(11):37-43.
16. Lee JM, Kim YJ. Foreign body granulomas after the use of dermal fillers: pathophysiology, clinical appearance, histologic features, and treatment. Arch Plast Surg. 2015;42(2):232-9.
17. Beleznay K, Humphrey S, Carruthers JD, Carruthers A. Vascular compromise from soft tissue augmentation: experience with 12 cases and recommendations for optimal outcomes. J Clin Aesthet Dermatol. 2014;7(9):37-43.
18. Claudio D. New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events. Aesthetic Surgery Journal. 2017.
19. Walker L, Convery C, Davies E, Murray G, Croasdell B. Consensus Opinion for The Management of Soft Tissue Filler Induced Vision Loss. J Clin Aesthet Dermatol. 2021;14(12):E84-e94.
20. Halepas S, Chen XJ, Ferneini EM. Thread-Lift Sutures: Anatomy, Technique, and Review of Current Literature. J Oral Maxillofac Surg. 2020;78(5):813-20.
21. Niu Z, Zhang K, Yao W, Li Y, Jiang W, Zhang Q, et al. A Meta-Analysis and Systematic Review of the Incidences of Complications Following Facial Thread-Lifting. Aesthetic Plast Surg. 2021;45(5):2148-58.
22. Sarigul Guduk S, Karaca N. Safety and complications of absorbable threads made of poly-L-lactic acid and poly lactide/glycolide: Experience with 148 consecutive patients. J Cosmet Dermatol. 2018;17(6):1189-93.
23. Isaac J, Henderson A. Avoiding Thread Lifting Complications. The Aesthetics Journal. 2023;10.
24. Wang CK. Complications of thread lift about skin dimpling and thread extrusion. Dermatol Ther. 2020;33(4):e13446.
25. Chen Y, Niu Z, Jin R, Lei Y, Han Y. Treatment of Complications following Facial Thread-Lifting. Plast Reconstr Surg. 2021;148(1):159e-61e.
26. Rezaee Khiabanloo S, Nabie R, Aalipour E. Outcomes in thread lift for face, neck, and nose; A prospective chart review study with APTOS. J Cosmet Dermatol. 2020;19(11):2867-76.

